DNP 820 10 Strategic Points Documents for Quality Improvement Project
Sample Answer for DNP 820 10 Strategic Points Documents for Quality Improvement Project Included After Question
The purpose of this assignment is to outline the 10 strategic points that defne the intended research focus and approach.
In the DPI Project, there are 10 strategic points that need to be clear, simple, and aligned to ensure that the resulting research is valuable and credible. These key points, which emerge over the course of the research process, will provide a guiding vision for the DPI Project.
Page 23 Grand Canyon University 2022 © Prepared on: Jan 12, 2022
General Requirements:
Use the following information to ensure successful completion of the assignment:
Refer to the “10 Strategic Points A Courses” resource located in the DC Network to complete this
assignment.
Doctoral learners are required to use the current APA style for their essay writing assignments. The current
APA Style Guide is located in the Student Success Center.
This assignment uses a rubric. Please Review the rubric prior to the beginning to become familiar with the
expectations for successful completion.
You are required to submit this assignment to LopesWrite. A link to the LopesWrite technical support
articles is located in Class Resources if you need assistance.
Directions:
Draft statements for each of the 10 strategic points for your intended project, incorporating feedback received
on past submissions of the 10 Strategic Points document in previous courses. This assignment is not a paper
and should be developed and submitted in a table format.
Benchmark Information:
This benchmark assignment assesses the following programmatic competencies:
DNP
1.2: Apply science-based theories and concepts to determine the nature and signifcance of health and health care
delivery phenomena.
1.3: Employ science-based theories and concepts to describe the actions and advanced strategies to enhance,
alleviate, and ameliorate health and health care delivery phenomena as appropriate.
4.2: Synthesize concepts to develop, implement, and evaluate interventions to improve individual, aggregate
population health management.
A Sample Answer For the Assignment: DNP 820 10 Strategic Points Documents for Quality Improvement Project
Title: DNP 820 10 Strategic Points Documents for Quality Improvement Project
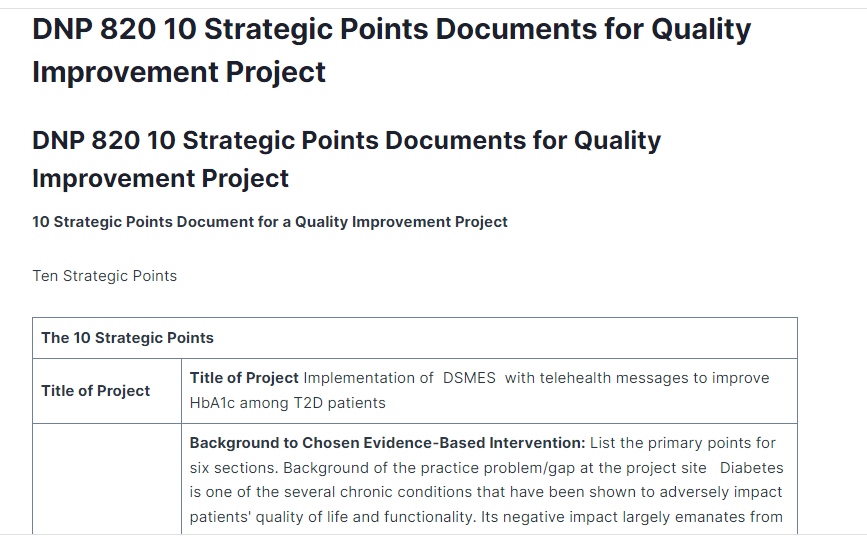
Ten Strategic Points
| The 10 Strategic Points | |
| Title of Project | Title of Project Implementation of DSMES with telehealth messages to improve HbA1c among T2D patients |
| Background Theoretical Foundation Literature Synthesis Practice Change Recommendation | Background to Chosen Evidence-Based Intervention: List the primary points for six sections. Background of the practice problem/gap at the project site Diabetes is one of the several chronic conditions that have been shown to adversely impact patients’ quality of life and functionality. Its negative impact largely emanates from potential conditions which may result due to diabetes, such as stroke, heart disease, kidney disease, and blindness (Skinner et al.,2020). Diabetes impacts millions of life, limiting their ability to lead normal lives and prompting a need to come up with better strategies to prevent, manage and treat the condition (Zhang et al., 2020). Even though various approaches have been applied in efforts to minimize the adverse impacts of the condition, diabetes still ranks high among the most disabling and prevalent diseases (Zakin et al., 2019). Recent statistics showed that the world’s diabetes prevalence stands as high as close to 10% (Khan et al., 2019). Due to its chronic nature, the major interventions used in managing patients with diabetes aim at ensuring that the patients have better patient outcomes relative to factors such as glycemic control and reducing the indulgence in risky lifestyle behaviors. Such risky lifestyle behaviors have a huge potential to negatively impact the appropriate management of the disease (Maiorino et al., 2020). Even though the normal strategies have been applied at the practice site, the outcomes have not been as desired as patients still present with poorly controlled HbA1c, which exposes them to other comorbidities. As such, there is a need to focus more on diabetes management and apply more robust strategies that can help the patient better manage their HbA1c levels. Diabetes self-management education and support have been shown to improve diabetes-related patient outcomes (Azami et al., 2018). In addition, with the advancement of technology, integrating aspects like telehealth with DSMES is proving to be more promising in terms of helping patients with diabetes have better HbA1c and other diabetes-related outcomes (Nelson et al.,2021). However, the use integration of telehealth aspects such as telehealth messages is still minimal or absent in some practice settings such as the practice site. Therefore it is expected that improved patient outcomes will be the result of the integration of DSMES and telehealth messages. Significance of the practice problem/gap at the project site The chronic nature of diabetes means that the patients have to spend a lot of money yearly to ensure improved outcomes. As such, there have been efforts to use more robust approaches, such as leveraging technological advancements to formulate better diagnosis, prevention, management, and treatment strategies (Teymourian et al.,2020). Nonetheless, individuals who are diagnosed with the condition annually are millions, while many others die yearly (Khan et al.,2019). As such, nursing has a role to play in coming up with appropriate nursing interventions which can be used to improve diabetes management, such as integrating DSMES with telehealth messages. Such strategies can go a long way toward helping the patient develop better self-management strategies to improve diabetes-related outcomes such as HbA1c levels. This is significant to the practice site as positive outcomes would mean that the practice site will develop the use of DSMES with telehealth as the standard diabetes management strategy. The implication is that the practice site will need to adopt this strategy to help improve patients’ HbA1c; on the contrary, failure to address the problem would mean that patients with diabetes would continue having poorly controlled HbA1c hence poorer health outcomes. Theoretical Foundations (choose one nursing theory and one evidence-based change model to be the foundation for the project): Nursing theories are important in guiding nursing interventions focused on improving patient outcomes since, through their frameworks, facets of proposed interventions can appropriately be implemented. Therefore, the nursing theory chosen to guide this project is Dorothea Orem’s self-care theory; the major claim of the theory involves assisting others by giving them and maintaining self-care with the major focus of improving the individual’s home-level effectiveness and functioning. Orem argued that every individual is capable of performing self-care, which entails a host of activities that the person starts to maintain their well-being, health, and life (Butts & Rich, 2018). This theory is composed of three major supporting sub-theories. They include the theory of nursing systems, the self-care deficit theory, and the theory of self-care (Orem & Calnan, 1972). The theory will be used as a supporting theory in the implementation of the DNP project on diabetes management. As earlier indicated, the chronic nature of diabetes requires that individuals undertake self-management activities for better outcomes. Therefore, the theory supports actions to be taken by the individuals, such as performing actions learned through educational initiatives and attending to the self-care needs for better outcomes. According to the theory, self-care is more natural to adults and can be taught; as such, this underpinning will be key in guiding the DNP project in the promotion of self-care and self-maintenance among patients living with diabetes through the DSMES integrated with telehealth messages. Another aspect of the theory is that it indicates the possibility of the patients and the caregivers having deficits in terms of sufficient information and resources. For example, the patient’s inability to undertake self-care makes them in need of support. This theory helps the project by linking what the patients need to do for better outcomes. This, therefore, fits the use of the proposed intervention to help the patients have better outcomes. Participating in the telehealth-supported diabetes self-management education program will ensure that the patients have a diminished incidence of emergency room visits. Evidence-based change models are also important in patient intervention projects or initiatives as they help in the appropriate management of the change. As such, Kurt Lewin’s change theory was chosen to be used as part of this DNP project. The theory will be key in addressing the stakeholder concerns, attitudes, and fears. This theory has three major phases which can be used in guiding a change initiative. The three stages include unfreezing, change, and refreezing phases (Lewin, 1947). In addition, the theory states that during a change process, there are two predominant forces; the restraining and the driving forces, which bar change and foster change, respectively. As such, a change can only occur successfully when the driving forces overcome the restraining forces. The first phase of the theory is the unfreezing stage, where an urgent need or urge for change is created (Hussain et al.,2018). This stage helps the project by linking the urgent need for change and ensuring that the patients and the nurses see the urgent need to improve their patient’s HbA1c levels. Therefore, the nurses will help the patient see the need to use more effective strategies to improve their HbA1c levels hence the importance of participating in the project. The change stage involves implementing the proposed change, which involves rolling out the DSMES integrated with telehealth messages to help improve outcomes. The third stage, which is the refreezing stage, will entail making use of the intervention to be part and parcel of the normal management strategy at the practice site. As such, the healthcare professionals involved in diabetes management will be required to use the intervention and support the patients for improved outcomes. Annotated bibliography Nelson, L. A., Greevy, R. A., Spieker, A., Wallston, K. A., Elasy, T. A., Kripalani, S., … & Mayberry, L. S. (2021). Effects of a tailored text messaging intervention among diverse adults with type 2 diabetes: evidence from the 15-month REACH randomized controlled trial. Diabetes Care, 44(1), 26–34. https://doi.org/10.2337/dc20-0961 The major aim of this study was to examine the efficacy of tailored text messages addressing medication adherence and self-care behaviors among patients with diabetes in improving their HbA1c levels. This study, known as Rapid Education and Communication for Health (REACH), was a randomized controlled trial performed in Tennessee, USA. A total of 506 participants were recruited in the study, with 253 randomized into the control group while 253 were in the intervention group (REACH). The intervention group was further randomized into the REACH-only group (127) or REACH with Family-Focused Add-on for Motivating Self-care (FAMS)- 126. The intervention group was offered monthly phone coaching delivered through text messages regarding self-care. Upon the use of the intervention, the HbA1c levels among the intervention group were found to reduce more than the intervention group (p=0.049) at six months of the study. Fortmann, A. L., Gallo, L. C., Garcia, M. I., Taleb, M., Euyoque, J. A., Clark, T., … & Philis-Tsimikas, A. (2017). Dulce Digital: an mHealth SMS-based intervention improves glycemic control in Hispanics with type 2 diabetes. Diabetes Care, 40(10), 1349–1355. https://doi.org/10.2337/dc17-0230 Fortmann et al’s. (2019) research had the main aim of examining the efficacy of text messaging in delivering diabetes care messages among patients with diabetes in lowering the HbAlc levels. This was a randomized controlled trial performed in California, United States. A total of 126 patients with poorly controlled diabetes were recruited, with 63 randomized into the intervention group while the remaining were randomized into the control group. The intervention group received text messages with calls detailing a culturally appropriate DSME. The messages were sent two to three times a day for six months. The control group only watch videos on diabetes management at the start of the study. At baseline, both groups had poor glycemic control. Upon the use of the intervention, the intervention group showed a greater reduction in HbA1c both at three months (p=0.03)and six months (p=0.03) as compared to the control group Dobson, R., Whittaker, R., Jiang, Y., McNamara, C., Shepherd, M., Maddison, R., … & Murphy, R. (2020). Long‐term follow‐up of a randomized controlled trial of a text‐message diabetes self‐management support program, SMS4BG. Diabetic Medicine, 37(2), 311–318. https://doi.org/10.1111/dme.14182 This research was carried out with the major aim of examining the efficacy of individually tailored text-message diabetes self-management support programs on patients’ HbA1c levels among patients with type 2 diabetes. The study was conducted in New Zealand. This was also a randomized controlled trial where a total of 293 patients were included in the study, with 177 randomized into the intervention group while 116 were randomized into the control group. The intervention group received automated text-messages self-management support on how to successfully manage diabetes. At the end of the study, there was a bigger reduction in HbA1c levels among the intervention group as compared to the control group (p<0.0001), showing the efficacy of the intervention. Vinitha, R., Nanditha, A., Snehalatha, C., Satheesh, K., Susairaj, P., Raghavan, A., & Ramachandran, A. (2019). Effectiveness of mobile phone text messaging in improving glycaemic control among persons with newly detected type 2 diabetes. Diabetes Research and Clinical Practice, 158, 107919. https://doi.org/10.1016/j.diabres.2019.107919 Vinitha et al. (2019) conducted a study with the aim of evaluating the impact of text messaging in improving glycemic control among patients with type 2 diabetes. This was a multicenter randomized controlled trial study conducted in India. The researchers recruited a total of 248 patients, where 122 were randomized into the control group, and 126 were randomized into the intervention group. While the control group was offered the standard care, the intervention group received care supported with customized text messages three times a week. The analysis of the data showed that the intervention was efficacious. Both group groups had a significant drop in HbA1c levels (p<0.0001). However, the reduction observed in the intervention group was greater than that of the control group (p=0.044) Riangkam, C., Sriyuktasuth, A., Pongthavornkamol, K., Kusakunniran, W., & Sriwijitkamol, A. (2021). Effects of a mobile health diabetes self-management program on HbA1C, self-management and patient satisfaction in adults with uncontrolled type 2 diabetes: a randomized controlled trial. Journal of Health Research, (ahead-of-print). https://doi.org/10.1108/JHR-02-2021-0126 The aim of this study was to determine the impact of a mobile health diabetes program (MHDSMP) intervention on diabetes self-management behavior and outcomes among patients with type 2 diabetes. This study was conducted in Thailand and was a three-arm parallel group randomized controlled trial. A total of 129 patients were recruited to take part in the study. Forty-three participants were randomized in each of the three groups; MHDSMP, telephone follow-up, and usual care. The intervention received diabetes management through text messages and telephone coaching. The study went on for three months, and by the end of the study, analysis of the data showed that there was a statistically significant reduction in HbA1c levels in the intervention group (p<0.001) Practice Change Recommendation: Validation of the Chosen Evidence-Based Intervention The usual care approaches have been applied at the practice site to manage patients with diabetes. However, patients continue to have undesirable effects, such as poor glycemic control. Therefore, this project proposes the use application of a DSMES integrated with telehealth text messages to help patients have well-controlled HbA1c levels, as indicated in research done by Nelson et al. (2021). In this research, a randomized controlled trial was used, and the patients in the intervention group who had diabetes education supported with telehealth messages had a greater reduction in HbA1c levels ((p=0.049) at six months). The results show that the intervention used by Nelson et al. (2021) is effective in reducing patients’ HbA1c levels hence a recommendation for practice change from the usual care to telehealth-supported DSMES. Summary of the findings written in this section. The adverse impacts of diabetes as a chronic condition mean that various researchers have embarked on finding the best solutions to the condition. From the research articles in the annotated bibliography, it has been shown that the use of telehealth-supported DSMES improves patients’ HbA1c levels. In all the articles, a comparison in HbA1c levels between the intervention groups and control groups revealed that the intervention groups experienced a more significant reduction in the HbA1c levels; for instance, Nelson et al. (2021) observed a statistically significant difference (p=0.049), Fortmann et al. (2017); p=0.03, Dobson, et al. (20200; p=0.0001, Vinitha et al. (2019); p=0.004 and Riangkam et al.(2020); p=0.001 |
| Problem Statement | Problem Statement: Describe the variables/groups to project in one sentence. It is not known if the implementation of DSMES with telehealth messages would impact Hb1Ac levels among patients with type 2 diabetes. |
| PICOT to Evidence-Based Question | PICOT Question Converts to Evidence-Based Question: Among patients with type 2 diabetes in a nursing home, will the translation of Nelson et al’s research on diabetes self-management education and support with telehealth messages compared to the current practice improve patient HbA1c levels in 12 weeks? Evidence-Based Question: Provide the templated statement To what degree will the implementation of Nelson et al’s research on diabetes self-management education and support with telehealth messages impact HbA1c levels among patients with type2 diabetes in a large city nursing home? |
| Sample Setting Location Inclusion and Exclusion Criteria | Sample, Setting, Location Identify the sample, needed sample size, and location (project phenomena with small numbers and variables/groups with large numbers). Sample and Sample Size: The sample will be obtained through convenient sampling, where a total of 30 patients with type 2 diabetes will be recruited to take part in the study. A sample calculator is to be used to get the correct number of participants. One of the possible biases is selection bias, as patients to participate in the study are ones known to the nursing home. There is a potential for lack of generalizability as patients will be drawn from a single center.Setting: the setting is a nursing homeLocation: The nursing home is located in a large city in the USAInclusion CriteriaWho can participate? The patients must be adults (at least 18 years of age) and have type 2 diabetes. Should not be part of another chronic disease study. The patients should be willing to take part in the study to be considered. Exclusion CriteriaWho cannot participate: patients under the age of 18 years will be excluded, and patients who are already participating in another study will be excluded. Patients who are unwilling to take part will also be excluded |
| Define Variables | Define Variables:Independent Variable (Intervention): diabetes self-management education and support with telehealth messagesDependent Variable (Measurable patient outcome): HbA1c levels |
| Project Design | Project Design: This project will use a quality improvement approach. You must be able to explain and cite the difference between research and quality improvement (one paragraph each). Quality Improvement: quality improvement refers to a project or initiative aiming at improving patient outcomes. They are formulated to help minimize the chances of errors and improve patient outcomes. They are also started to help fill care gaps that have been observed in the patient care strategies. Application of quality improvement in this project will consider existing research and translate the best evidence to help improve HbA1c levels among patients with type 2 diabetes in the practice site. In contrast to research, quality improvement involves the application of the already existing evidence to boost patient outcomes.Research: Research is a process of coming up with new ideas or knowledge to improve the current knowledge and standards of practice. It involves a systematic study of an existing problem or a clinical concern and coming up with hypotheses which are then tested to yield novel knowledge (Glasofer & Townsend). The importance of research emanates from the fact that it helps in producing scholarly evidence. Such evidence is applied in formulating guidelines and standards for nursing practice. Research is also used to come up with quality improvement efforts and initiatives.Summarize Both quality improvement and research are key in patient care as they both focus on improving patient outcomes. Nonetheless, the two are distinct from each other. Research focuses on new knowledge creation as well as coming up with new theories. Quality improvement translates the findings from research into practice. |
| Purpose Statement | Purpose Statement: Provide the templated statement. The purpose of this quality improvement project is to determine if the implementation of diabetes self-management education and support with telehealth messages would impact HbA1c levels among patients with type 2 diabetes. The project was piloted over an eight-week period in an urban nursing home. |
| Data Collection Approach | Data Collection Approach:A RedCap database will be applied to measure the patient information. The baseline characteristics and demographic data, such as the patient’s comorbidities, ethnicity, race, age, and gender, will all be recorded for every participant. The baseline HbA1c data for the patients will be obtained from the facilities, electronic health records.The Redcap database will be used to enter all the information related to the patient. The patientThe collected data will be protected from unauthorized access using the pass-worded RedCap database. Access will only be granted to those who have the provided secret password. In addition, a number will be assigned to every medical record as a way of de-identification.Step-by-step process of data collectionThe baseline HbA1c level data for the participants will be obtained from the facility’s EHRThe patients will use phones to receive interactive text messages on diabetes management.The patients will be expected to send back text messages if they have understood the contents of what has been sent.The HbA1c levels will be measured at the end of the intervention, and the data will be entered into the RedCap database. Various steps will be taken to ensure that the patient’s rights are not infringed, and the data remains confidential. Participation will remain open and voluntary, as no patient will be coerced. The data will be de-identified, while the database with the patient data will be password protected. The data will be stored for one year after graduation, followed by disposal to protect patients further.This project also intends to follow the Belmont principles. Hence, it will ensure that harm is prevented. Participation will also remain totally voluntary. The patients will also be treated with respect while respecting their autonomy. |
| Data Analysis Approach | Data Analysis Approach:The data will be analyzed using suitable software. Central measures of tendency, such as average, mean, and median, will be applied to summarize the patient’s characteristics. Descriptive statistics will be used to analyze the demographic data, the mean, median and standard deviations.While some data will be obtained from the EHR, the project data for comparison will be measured by the nurses, and comparison will be made to determine the efficacyPaired sample t-test will be used to obtain the differences between pre and post-interventionA statistician will be used in the statistical analysis and appropriate interpretation. Various biases are expected in this project. For example, in case a positive effect is observed, there could be a possibility that such results may not be all down to the intervention. Therefore, as a way of mitigating this, a study design will be used to ensure that the patients only used the indicated intervention. |
| References | Azami, G., Soh, K. L., Sazlina, S. G., Salmiah, M., Aazami, S., Mozafari, M., & Taghinejad, H. (2018). Effect of a nurse-led diabetes self-management education program on glycosylated hemoglobin among adults with type 2 diabetes. Journal of diabetes research, 2018. https://doi.org/10.1155/2018/4930157 Butts, J. B., & Rich, K. L. (2018). Philosophies and theories for advanced nursing practice. Jones & Bartlett Publishers. Dobson, R., Whittaker, R., Jiang, Y., McNamara, C., Shepherd, M., Maddison, R., … & Murphy, R. (2020). Long‐term follow‐up of a randomized controlled trial of a text‐message diabetes self‐management support program, SMS4BG. Diabetic Medicine, 37(2), 311–318. https://doi.org/10.1111/dme.14182 Fortmann, A. L., Gallo, L. C., Garcia, M. I., Taleb, M., Euyoque, J. A., Clark, T., … & Philis-Tsimikas, A. (2017). Dulce Digital: an mHealth SMS-based intervention improves glycemic control in Hispanics with type 2 diabetes. Diabetes Care, 40(10), 1349–1355. https://doi.org/10.2337/dc17-0230 Glasofer, A., & Townsend, A. B. (2021). Determining the level of evidence. Nursing, 51(2), 62–65. https://doi.org/10.1097/01.nurse.0000731852.39123.e1 Hussain, S. T., Lei, S., Akram, T., Haider, M. J., Hussain, S. H., & Ali, M. (2018). Kurt Lewin’s change model: A critical review of the role of leadership and employee involvement in organizational change. Journal of Innovation & Knowledge, 3(3), 123-127. https://doi.org/10.1016/j.jik.2016.07.002 Maiorino, M. I., Signoriello, S., Maio, A., Chiodini, P., Bellastella, G., Scappaticcio, L., … & Esposito, K. (2020). Effects of continuous glucose monitoring on metrics of glycemic control in diabetes: a systematic review with meta-analysis of randomized controlled trials. Diabetes Care, 43(5), 1146-1156. https://doi.org/10.2337/dc19-1459 Nelson, L. A., Greevy, R. A., Spieker, A., Wallston, K. A., Elasy, T. A., Kripalani, S., … & Mayberry, L. S. (2021). Effects of a tailored text messaging intervention among diverse adults with type 2 diabetes: evidence from the 15-month REACH randomized controlled trial. Diabetes Care, 44(1), 26–34. https://doi.org/10.2337/dc20-0961 Orem, D. E., & Calnan, M. E. (1972). NURSING. Nursing Management (Springhouse), 3(1), 43-46. https://doi.org/10.1097/00006247-197201000-00013 Skinner, T. C., Joensen, L., & Parkin, T. (2020). Twenty‐five years of diabetes distress research. Diabetic Medicine, 37(3), 393-400. https://doi.org/10.1111/dme.14157. Teymourian, H., Barfidokht, A., & Wang, J. (2020). Electrochemical glucose sensors in diabetes management: An updated review (2010–2020). Chemical Society Reviews, 49(21), 7671–7709. https://doi.org/10.1039/D0CS00304B Zakin, E., Abrams, R., & Simpson, D. M. (2019, October). Diabetic neuropathy. In Seminars in neurology (Vol. 39, No. 05, pp. 560–569). Thieme Medical Publishers. DOI: 10.1055/s-0039-1688978 Zhang, Y., Lazzarini, P. A., McPhail, S. M., van Netten, J. J., Armstrong, D. G., & Pacella, R. E. (2020). Global disability burdens of diabetes-related lower-extremity complications in 1990 and 2016. Diabetes Care, 43(5), 964–974. https://doi.org/10.2337/dc19-1614 |
A Sample Answer For the Assignment: DNP 820 10 Strategic Points Documents for Quality Improvement Project
Title: DNP 820 10 Strategic Points Documents for Quality Improvement Project
10 Strategic Points Document for a Quality Improvement Project
Ten Strategic Points
| The 10 Strategic Points | |
| Title of Project | Title of Project Using continuous glucose monitoring to monitor blood glucose in adult patients with type II diabetes |
| Background Theoretical Foundation Literature Synthesis Practice Change Recommendation | Background to Chosen Evidence-Based Intervention: List the primary points for six sections Background of the practice problem/gap at the project site Several chronic conditions negatively impact the lives of patients. Among such conditions is diabetes. Diabetes causes numerous other complications, such as kidney disease, heart disease, and stroke (Skinner et al., 2020). The other concern about diabetes is that it affects millions of people, making them unable to live normal lives. The implication is that various researchers and stakeholders have, in the past and present, been pursuing effective ways or strategies to better manage diabetes. Non-the less, diabetes is still among the most prevalent chronic conditions (Khan et al., 2019). According to Khan et al. (2019) the diabetes global prevalence among the adult population is as high as 9%. The interventions currently in use among patients living with diabetes majorly focus on helping patients attain better healthcare outcomes, such as better glycemic control and keeping in check the risky lifestyle behaviors that may hinder the control and management of the condition (Maiorino et al., 2020). Even though effective interventions should be applied, the management strategies used in the practice site have not achieved the desired results as most of the patients fail to achieve the required HbA1c levels. Indeed, uncontrolled levels of HbA1c have been connected to myocardial infarction and stroke disease (Azhar et al., 2022). It hurts to use an invasive glucometer. The discomfort is the same even if the needle is very small. Some individuals may be able to adjust to it and tolerate it, but for others, it may be too much to handle, leading to the issue of non-compliance. The patient’s ability to regulate their blood sugar may suffer as a result, leading to bouts of hyperglycemia and hypoglycemia The risk of diabetic complications is increased by noncompliance, making it a potentially life-threatening issue, hence the need to have a different way to measure glucose more effectively and non-invasively. Significance of the practice problem/gap at the project site As earlier highlighted, diabetes causes other undesirable problems apart from making those who live with it spend more money on treatment and management (Bommer et al., 2018). Therefore, the need to control and manage the disease has attracted the attention of several stakeholders, including nurses, doctors, and other researchers in the medical and nursing fields. There have been advancements in the management of diabetes, largely due to the new innovative technologies used in diagnostics and treatment (Haque et al., 2021). However, the annual number of people who get the disease still runs into millions. In addition, the prevalence rates have been rising in recent years, while several others die annually due to diabetes (Khan et al., 2019). The negative impacts caused by the disease can reduce through using nursing interventions based on the current technology and technological applications such as continuous glucose monitoring. The intervention can dictate the rate of practitioners ordering Continuous glucose monitoring as directed by the results to further improve outcomes. The implication is that, in the event that continuous glucose monitoring leads to improvement in the expected HbA1c levels, then the practitioners at the project site are more likely to increase the rates of the ordering of continuous glucose monitoring for better outcomes (Root et al., 2022). Modern intensive diabetic care relies on regular and precise monitoring of blood glucose levels. This used to require many time-consuming and uncomfortable daily random blood glucose readings, which served as a substantial deterrent to reaching intended blood glucose targets. Self-monitoring blood glucose (SMBG) simply gives you a single reading of the blood sugar level and doesn’t tell user anything about the trend or pace of the sugar levels even if used consistently. This means that most individuals, notwithstanding the checking their glucose concentration multiple times a day, nonetheless fail to meet their goals. CGM is a major improvement because it offers immediate evaluation on the efficacy of diabetic therapies (such insulin delivery), and it gives alerts when serum sugar levels reach critically excessive or inadequate. more importantly, it offers real-time glucose reading at regular intervals. This is significant to the research, since benefits of CGM out do the shortcomings, which include high cost. Theoretical Foundations (choose one nursing theory and one evidence-based change model to be the foundation for the project): Nursing theories are key in implementing nursing interventions as they offer a framework upon which to base the aspects of interventions (Brandão et al., 2019). Therefore, this project will use Dorothea Orem’s self-care theory. The theory is mainly defined as the act of helping others by offering and maintaining self-care to maintain and improve human functioning at the home level effectiveness. The theory states that an individual has an ability to perform self-care as “the practice of activities that individuals initiate and perform on their behalf to maintain life, health, and well-being (Butts & Rich, 2018). Dorothea’s theory has three interconnected sub-theories; the theory of self-care, the self-care deficit theory, and the theory of nursing systems (Orem & Calnan, 1972). Dorothea Orem’s theory is one of the nursing theories widely applied in nursing quality improvement and change initiatives. This theory will be used in guiding the DNP project on diabetes management and prevention. Self-care is key in diabetes management. Therefore, the underpinnings will be key in helping the individuals evaluate themselves and choose the necessary actions required to attend to the needs of self-care by accomplishing the actions (Butts & Rich, 2018), which in this case is continuous glucose monitoring. Therefore, patients can be motivated to follow the interventions for better care. The theory underlines that self-care is learned and is more natural to adults. Therefore, it will guide the project toward promoting self-care for healthcare, well-being, and self-maintenance among the identified patients living with diabetes. The theory is also appropriate for the management of diabetes as it also focuses on the possible deficits that the caregivers or the patients may be having in terms of appropriate resources and information key to better management (Orem & Calnan, 1972). In addition, the theory also highlights the inability of patients to take care of themselves, hence the need for support. The patients will, therefore, be able to lower the chances of emergency room visits by taking instructions on the use of continuous glucose monitoring. The use of continuous glucose monitoring also focuses on self-care as the patients will be required to use the monitors, and the existence of a deficit will be a springboard to help the caregivers to collaborate and offer the best to achieve the set goals. Another aspect of the theory is the application of innovative and creative ideas (Orem & Calnan, 1972). Such ideas are key if the evidence is to be used to positively impact patient outcomes. As such, upon the improvement of patient outcomes through glucose monitoring, the impact and the next set of goals will be communicated to the care teams to help facilitate the new practice with the major focus of improving patient outcomes. Lewin’s change theory will provide the theoretical foundation and constructs in the change practice by addressing behaviors, fears, anxieties, and attitudes and reducing stakeholder worries. Kurt Lewin’s change theory comprises three stages, unfreezing, change, and refreezing (Lewin, 1947); (Hussain et al., 2018). The theory asserts that there are two types of forces, the driving and restraining forces pushing in the direction that makes change happen and the direction that hinders the change, respectively (Lewin, 1947). A change only occurs when the driving forces override the restraining forces (Cummings et al., 2016). In the unfreezing stage, a method is proposed to help individuals move from old behavior patterns and accept change. The change or moving stage entails changing behavior, feeling, and thoughts. The final step, refreezing, entails making the new change as a new habit or standard (Lewin, 1947). When applying the change model, the unfreezing stage will involve asserting the need for patients to have improved HbA1c levels hence the need for more effective intervention. During this stage, the nurses involved will ensure that the patients see the urgency of the need to have well-controlled HbA1c levels. The second step will involve implementing the proposed intervention to reduce HbA1c levels in diabetic patients. Support is offered to nurses who offer the intervention to patients, and the patients are encouraged to adhere to the intervention requirements. At this stage, the intervention is rolled out, and the patients are encouraged to use continuous glucose monitoring. The final step will involve making the intervention part of standard practice to ensure that patients have better outcomes. Therefore, nurses will be advised to apply the intervention to patients with diabetes for better diabetes outcomes. Besides, ordering continuous glucose monitoring by the practitioners will be expected to be the standard part of the diabetes management practices at the facility. Annotated bibliography. Beck, R. W., Riddlesworth, T. D., Ruedy, K., Ahmann, A., Haller, S., Kruger, D., … & DIAMOND Study Group. (2017). Continuous glucose monitoring versus usual care in patients with type 2 diabetes receiving multiple daily insulin injections: a randomized trial. Annals of Internal Medicine, 167(6), 365–374. DOI: 10.7326/M16-2855. In this study by Beck et al. (2017), the primary aim was to determine the effectiveness of continuous glucose monitoring in adults with type 2 diabetes who were getting insulin injections. By employing a randomized controlled trial as the research design, these researchers recruited one hundred and fifty-eight patients with type 2 diabetes. Seventy-nine patients were randomized into the usual care group, with the remaining half recruited into the intervention group. While the continuous glucose monitoring group used a Dexcom G4 platinum continuous monitoring system to monitor their glucose concentrations, the control groups engaged in glucose self-monitoring. The mean HbA1c levels went down to 7.7 % and 8.0% in the continuous glucose monitoring group and control group, respectively (adjusted difference in mean change, −0.3% [95% CI, −0.5% to 0.0%]; p = 0.022), showing that the intervention was efficacious. When continuous glucose monitoring was performed, there was a statistically significant decrease in HbA1c levels among the patients in the intervention groups. As a result, it suggests that continuous glucose monitoring is essential for enhancing diabetic outcomes like lowered HbA1c levels. Gilbert, T. R., Noar, A., Blalock, O., & Polonsky, W. H. (2021). Change in hemoglobin A1c and quality of life with real-time continuous glucose monitoring use by people with insulin-treated diabetes in the landmark study. Diabetes Technology & Therapeutics, 23(S1), S-35. https://doi.org/10.1089/dia.2020.0666 The study by Gilbert et al. (2021) aimed to assess the changes in HbA1c levels upon using a continuous glucose monitoring system. The recruited patients were two hundred and forty-eight, with sixty having Type 2 Diabetes.The participants were requested to upload their point-of-care HbA1c measurements to an online portal. They then used continuous glucose monitoring devices to monitor their HbA1c values and uploaded them to the portal. Upon data analysis, the researchers noted that there was a significant reduction in the levels of HbA1c levels (p-value <0.001). The HbA1c fell significantly from 8.2% (1.9%) at baseline to 7.1% (1.1%) at the end of the study (p < 0.001); besides, 54 % of those with initial HbA1c values >7% experienced absolute HbA1c reductions of >1%. This study implied that the improved HbA1c levels among the patients are the results of continuous glucose monitoring. Therefore, this study also indicated the importance of continuous glucose monitoring in improving HbA1c and the management of diabetes. Heinemann, L., Freckmann, G., Ehrmann, D., Faber-Heinemann, G., Guerra, S., Waldenmaier, D., & Hermanns, N. (2018). Real-time continuous glucose monitoring in adults with type 1 diabetes and impaired hypoglycemia awareness or severe hypoglycemia treated with multiple daily insulin injections (Hypo DE): a multicentre, randomized controlled trial. The Lancet, 391(10128), 1367-1377. https://doi.org/10.1016/S0140-6736(18)30297-6 This study was done by Heinemann et al. (2018). This study’s objective was to determine whether real-time continuous glucose monitoring can effectively reduce the severity and incidences of hypoglycemia. In a six-month randomized controlled study, the researchers randomly assigned 75 individuals to a real-time continuous glucose monitoring group, while 74 were assigned to the control groups. The individuals in the real-time continuous glucose monitoring group were taught how to use the monitoring system. They then used real-time continuous monitoring devices for the period of study. On the other hand, the individuals in the control group used glucometer to self-monitor their blood glucose levels at regular intervals during the day. Upon the analysis of the data, it was noted that the individuals in the intervention group reported a significant reduction in hypoglycemic events (p-value of <0.0001). The mean number of hypoglycemic events per month in the continuous glucose monitoring group was reduced from 10·8 (SD 10·0) to 3·5 (4·7); changes in the control group were not significant (from 14·4 [12·4] to 13·7 [11·6]). Incidence of hypoglycemic events decreased by 72% for participants in the continuous glucose monitoring group (incidence rate ratio 0·28 [95% CI 0·20–0·39], p<0·0001). The study implied that the use of continuous glucose monitoring led to a significant reduction in HbA1c levels hence showing the importance of the intervention in diabetes management and care. Martens, T., Beck, R. W., Bailey, R., Ruedy, K. J., Calhoun, P., Peters, A. L., … & MOBILE Study Group. (2021). Effect of continuous glucose monitoring on glycemic control in patients with type 2 diabetes treated with basal insulin: a randomized clinical trial. JAMA, 325(22), 2262-2272. doi:10.1001/jama.2021.7444 This article presents the findings of the research done by Martens et al. (2021). This study was done with the aim of finding the impacts of continuous glucose monitoring in improving individuals’ HbA1c levels when compared to the impact of blood glucose meter monitoring. In a randomized controlled trial, these researchers recruited a total of 175 people with type 2 diabetes. While the individuals in the intervention group used continuous glucose monitoring, the ones in the control group engaged in blood glucose meter monitoring. This study was done for a period of eight months. Upon analyzing the data, it was noted that the individuals in the intervention group showed a substantial reduction in HbA1c levels (p-value of 0.02). There was also a significant difference between the intervention and control groups (p-value of 0.001). Mean HbA1c level decreased from 9.1% at baseline to 8.0% at eight months in the continuous glucose monitoring group and from 9.0% to 8.4% in the control group (adjusted difference, −0.4% [95% CI, −0.8% to −0.1%]; p= 0.02). The results imply that continuous glucose monitoring leads to a more significant reduction in HbA1c levels, indicating that the intervention is effective. Grace, T., & Salyer, J. (2022). Use of Real-Time Continuous Glucose Monitoring Improves Glycemic Control and Other Clinical Outcomes in Type 2 Diabetes Patients Treated with Less Intensive Therapy. Diabetes Technology & Therapeutics, 24(1), 26-31. DOI: 10.1089/dia.2021.0212. Authored by Grace & Salyer (2022), this study focused on using real-time continuous glucose monitoring in the management of patients with diabetes type to improve glycemic control. The researchers recruited patients with type 2 diabetes with basal insulin only or noninsulin therapy. At six months, the researcher found relevant outcomes. For example, the participants showed a considerable reduction in HbA1c levels (−3.0% ± 1.3%, p-value <0.001). In addition, the researchers observed a reduction in the average levels of glucose at six months (−23.6 ± 38.8, P < 0.001). Therefore, continuous glucose monitoring was connected with significant glycemic improvements among patients with type 2 diabetes. Practice Change Recommendation: Validation of the Chosen Evidence-Based Intervention The standards of diabetes care have been used at the facility for years as a preference. However, this approach has not been as effective as expected. As such, this research proposes to investigate whether the increased prescription of continuous glucose monitoring as an intervention to help patients with type 2 diabetes have improved HbA1c levels, as shown in the research done by Beck et al. (2017). In a randomized controlled trial, the researchers randomized (n=79) patients in a continuous glucose monitoring group while (n=79) were in the control group. The continuous glucose monitoring group used a Dexcom G4 platinum continuous monitoring system to monitor their glucose concentrations to give a better reduction in HbA1c levels as compared to the control group (p values of 0.022). The analysis of the study findings showed that the mean HbA1c levels went down to 7.7 % and 8.0% in the continuous glucose monitoring group and control group, respectively (adjusted difference in mean change, −0.3% [95% CI, −0.5% to 0.0%]; P = 0.022), showing that the intervention was efficacious (Beck et al.,2017). As such, this randomized controlled trial study shows that continuous glucose monitoring can effectively improve HbA1c levels among patients with type 2 diabetes hence a recommendation for practice change (Beck et al., 2017). Summary of the findings written in this section. Diabetes is one of the most common and disabling chronic conditions. However, the application of nursing interventions can be key to improving patient outcomes (Beck et al., 2017). From the annotations, it is evident that the use of continuous glucose monitoring as an intervention in managing diabetes leads to a better control in patient’s blood glucose, even though the cost of purchasing it is significantly higher. For example, the researchers reported significant improvement in the HbA1c levels upon the use of continuous glucose monitoring. When the results for the control groups were compared with intervention groups, significant improvements among the intervention groups were observed. For example, the reduction in the HbA1 levels observed between the intervention and control group by Beck et al. (2017) was significant (p= 0.022); Gilbert et al. (2021) observed (p < 0.001), Heinemann et al. (2019) observed (p < 0.001); Martens et al. (2021) also observed (p < 0.001); Grace & Salyer observed (p <0.001) |
| Problem Statement | Problem Statement: Describe the variables/groups to project in one sentence. It is not known if the implementation of the translation of research by Beck et al. (2017) on continuous glucose monitoring to improve the rate of practitioners’ ordering continuous glucose monitoring would impact HbA1c levels among patients with type II diabetes. |
| PICOT to Evidence-Based Question | PICOT Question Converts to Evidence-Based Question: Among adult patients with type 2 diabetes in an outpatient clinic, will the translation of Beck et al.’s research on continuous glucose monitoring increase the rate of practitioners ordering continuous glucose monitoring impact HgbA1C compared to current practice in 12 weeks? Evidence-Based Question: Provide the templated statement. To what degree will the implementation of continuous glucose monitoring impact HbA1c levels among adult patients with type two diabetes in an urban outpatient clinic. |
| Sample Setting Location Inclusion and Exclusion Criteria | Sample, Setting, LocationSample and Sample Size: The sample will be based on a convenient sample of 16 adult patients diagnosed with type 2 diabetes. the sample will then be divided into two, the control group and the intervention group, each having 8 patients. One of the potential biases is selection bias, as the patients recruited will be ones known to the facility and attending the facility for the management of diabetes. Another potential bias is that the samples will be from one center, hence a lack of generalizability. The sample size of 16 patients is obtained by taking 10% of the total diabetic adults who visit the hospital, which is 160 patients Setting: The setting for the study is an urban Outpatient care primary clinic.Location: an outpatient primary care Clinic areaInclusion Criteria Patients must be at least 18 years and above and have type 2 diabetes. The patients should also be able to speak and understand English. The patient should also not form part of another study. The participants must be willing to participate in the study and must be competent in that they should be able make sound decisions on their own. Exclusion Criteria Patients under the age of 18 years will be excluded. Those who have other types of diabetes apart from type 2 diabetes will be excluded. Individuals using technological management of diabetes, those who do not want to sign the consent forms, and those who have a mental disability will be excluded. |
| Define Variables | Define Variables:Independent Variable (Intervention): continuous glucose monitoring Continuous glucose monitoring: Continuous glucose monitoring is a technological process of automatically tracking a person’s glucose concentrations throughout out the night and day. Dependent Variable (Measurable patient outcome): HbA1c levels Glucose concentrations: In reference to this project, blood glucose levels refer to the amount of the glucose in the patient’s system as measured by the continuous glucose monitors. HbA1c levels: In reference to this project, HbA1c levels refer to average glucose concentrations measured at baseline and at the end of the intervention to determine the efficacy of the intervention |
| Project Design | Project Design: This project will use a quality improvement approach. Quality Improvement: A quality improvement is an initiative or project focused on improving patient care efforts and outcomes. These initiatives focus on initiating changes to lower the chances of making medical errors, improving care, and ensuring safety. Quality improvement efforts also help formulate processes and standard work to bridge gaps for better patient outcomes. Quality improvement is vital in improving an organization’s performance and reducing costs. According to Fischer & Wick, 2020, quality improvement is key in delivering quality patient care composed of six aspects: patient-centered, equitable, timely, efficient, effective, and safe. Therefore, the use of the quality improvement approach in this study will seek to explore current research and translate the found evidence into practice for the major purpose of improving patient outcomes, which in this case is better HbA1c levels among patients with diabetes type 2. As opposed to research, quality improvement uses the existing evidence and translates the same into practice. Research: Research entails replicating or testing new ideas to improve the standard practice and current knowledge. A systematic strategy is applied to investigate a clinical question or problem, leading to the formulation of a hypothesis which then triggers efforts to prove such hypothesis and generate new knowledge (Glasofer & Townsend, 2021). Research is significant in nursing in that it produces scholarly evidence, which is then used as a guide to the professional nursing practice. Research differs from quality improvement in that it applies a systematic strategy to investigate a new idea and come up with new knowledge and theories. Therefore, research informs quality improvement. Summarize: Research and quality improvement both complement each other in terms of improving patient care outcomes. In addition, even though the two are connected, they are different. While research mainly formulates new knowledge, theories, and hypotheses, quality improvement focuses on translating the research findings into practice |
| Purpose Statement | Purpose Statement: Provide the templated statement. The purpose of this quality improvement project is to determine if the increased prescription of continuous glucose monitoring would impact HbA1c levels among adult patients with type 2 diabetes This project will be piloted over a twelve-week period in an urban Outpatient primary care clinic. |
| Data Collection Approach | Data Collection Approach: The demographic information or data for the patients, such as gender, co-morbidities, ethnicity, race, and age, will be collected. The demographic data for the patients will be collected through documentation during recruitment as provided by the patients. The patient’s knowledge of continuous glucose monitoring will also be evaluated using a questionnaire (Revised Brief Diabetes Knowledge Test instrument). The reliability of the Revised Brief Diabetes Knowledge Test instrument is (α ≥ 0.70), while the validity ranges from 0.83 to 0.96 The patient’s HbA1c levels will be measured, and the baseline data will be obtained from the electronic health records. Data from EHR has been shown to be reliable and valid. The obtained data at the end of the study period will then be entered into a password-protected database.The step-by-step process for collecting the data, Step 1: Obtaining IRB approval for data collection Step 2: Baseline patient HbA1c data will be obtained from the facility’s EHR. Step 3: The patient’s HbA1c will be measured after the intervention, and the two values will be compared. The results will also be compared between the intervention and the control group. Various potential ethical issues include the protection and storage of patient health information. This information will be stored in password-protected computers where only individuals with unique passwords will access the information. The patient data will also be de-identified to further improve security and confidentiality. In addition, the obtained data will be kept for one year after graduation before destroying them, following the Grand Canyon’s guidelines.The project will adhere to the principle of Belmont by ensuring that no harm is done to the patients. Patients will also be encouraged to participate in the study without coercion freely. Besides, none will be unfairly excluded from participating in the study. Patient data will also be protected to remain confidential and unauthorized access blocked. The patients will be shown the necessary respect in terms of autonomy and be treated without bias, just, fairly, and equally. |
| Data Analysis Approach | Data Analysis Approach:The participant’s data will be analyzed using the IBM SPSS statistics software. The central tendency measures will be used in summarizing the characteristics of the patients. They will be the mean or average of continuous and discrete data and the median.Descriptive statistics will be applied in analyzing the collected demographic data such as gender, co-morbidities, ethnicity, race, and age.Descriptive analysis will also be used to describe the population as well as what happens with the computation of standard deviations, median, and mean. It will also help in describing the variables and their relationships through the use of a mixed linear regression model.Data will be obtained from EHR and the continuous glucose monitoring database platform.There will be a review of the HbA1c levels obtained using continuous glucose monitors.Paired sample t-test and Pearson’s correlation will be used to determine the significant differences between the intervention data and baseline data and between the groups.A statistician will also be consulted to help with the statistical aspects of the project. Potential data bias can result in the possible improved glycemic control could be as a result of the intervention and other self-care activities that the patient undertakes outside the study. One way of mitigating data is through the use of an appropriate study design. The Hawthorne effect is also possible since the patients will be in the know that they are part of the study and, therefore, their behavior is being kept under watch |
| References | Azhar, S., Khan, F. Z., Khan, S. T., & Iftikhar, B. (2022). Raised Glycated Hemoglobin (HbA1c) Level as a Risk Factor for Myocardial Infarction in Diabetic Patients: A Hospital-Based, Cross-Sectional Study in Peshawar. Cureus, 14(6). Doi:10.7759/cureus.25723 Beck, R. W., Riddlesworth, T. D., Ruedy, K., Ahmann, A., Haller, S., Kruger, D., … & DIAMOND Study Group. (2017). Continuous glucose monitoring versus usual care in patients with type 2 diabetes, this is receiving multiple daily insulin injections: a randomized trial. Annals of Internal Medicine, 167(6), 365–374. https://doi.org/10.7326/M16-2855. Bommer, C., Sagalova, V., Heesemann, E., Manne-Goehler, J., Atun, R., Bärnighausen, T., … & Vollmer, S. (2018). Global economic burden of diabetes in adults: projections from 2015 to 2030. Diabetes care, 41(5), 963-970. https://doi.org/10.2337/dc17-1962 Brandão, M. A. G., Barros, A. L. B. L. D., Caniçali, C., Bispo, G. S., & Lopes, R. O. P. (2019). Nursing theories in the conceptual expansion of good practices in nursing. Revista Brasileira de Enfermagem, 72, 577-581. https://doi.org/10.1590/0034-7167-2018-0395 Butts, J. B., & Rich, K. L. (2018). Philosophies and theories for advanced nursing practice. Jones & Bartlett Publishers. Cummings, S., Bridgman, T., & Brown, K. G. (2016). Unfreezing change as three steps: Rethinking Kurt Lewin’s legacy for change management. Human relations, 69(1), 33–60. https://doi.org/10.1177/0018726715577707 Dang, D., Dearholt, S., Bissett, K., Ascenzi, J., & Whalen, M. (2022). Johns Hopkins evidence-based practice for nurses and healthcare professionals: model & guidelines. Sigma Theta Tau International Fischer, C., & Wick, E. (2020, November). An AHRQ national quality improvement project for implementation of enhanced recovery after surgery. In Seminars in Colon and Rectal Surgery (Vol. 31, No. 4, p. 100778). WB Saunders. https://doi.org/10.1016/j.scrs.2020.100778 Gilbert, T. R., Noar, A., Blalock, O., & Polonsky, W. H. (2021). Change in hemoglobin A1c and quality of life with real-time continuous glucose monitoring use by people with insulin-treated diabetes in the landmark study. Diabetes Technology & Therapeutics, 23(S1), S-35. https://doi.org/10.1089/dia.2020.0666 Glasofer, A., & Townsend, A. B. (2021). Determining the level of evidence. Nursing, 51(2), 62–65. https://doi.org/10.1097/01.nurse.0000731852.39123.e1 Grace, T., & Salyer, J. (2022). Use of Real-Time Continuous Glucose Monitoring Improves Glycemic Control and Other Clinical Outcomes in Type 2 Diabetes Patients Treated with Less Intensive Therapy. Diabetes Technology & Therapeutics, 24(1), 26-31. https://doi.org/10.1089/dia.2021.0212. Haque, W. Z., Demidowich, A. P., Sidhaye, A., Golden, S. H., & Zilbermint, M. (2021). The Financial Impact of an Inpatient Diabetes Management Service. Current Diabetes Reports, 21(2), 1-9. https://doi.org/10.1007/s11892-020-01374-0. Heinemann, L., Freckmann, G., Ehrmann, D., Faber-Heinemann, G., Guerra, S., Waldenmaier, D., & Hermanns, N. (2018). Real-time continuous glucose monitoring in adults with type 1 diabetes and impaired hypoglycemia awareness or severe hypoglycemia treated with multiple daily insulin injections (Hypo DE): a multicentre, randomized controlled trial. The Lancet, 391(10128), 1367-1377. https://doi.org/10.1016/S0140-6736(18)30297-6 Hussain, S. T., Lei, S., Akram, T., Haider, M. J., Hussain, S. H., & Ali, M. (2018). Kurt Lewin’s change model: A critical review of the role of leadership and employee involvement in organizational change. Journal of Innovation & Knowledge, 3(3), 123-127. https://doi.org/10.1016/j.jik.2016.07.002 Khan, R. M. M., Chua, Z. J. Y., Tan, J. C., Yang, Y., Liao, Z., & Zhao, Y. (2019). From pre-diabetes to diabetes: diagnosis, treatments, and translational research. Medicina, 55(9), 546. https://doi.org/10.3390/medicina55090546 Maiorino, M. I., Signoriello, S., Maio, A., Chiodini, P., Bellastella, G., Scappaticcio, L., … & Esposito, K. (2020). Effects of continuous glucose monitoring on metrics of glycemic control in diabetes: a systematic review with meta-analysis of randomized controlled trials. Diabetes Care, 43(5), 1146-1156. https://doi.org/10.2337/dc19-1459 Martens, T., Beck, R. W., Bailey, R., Ruedy, K. J., Calhoun, P., Peters, A. L., … & MOBILE Study Group. (2021). Effect of continuous glucose monitoring on glycemic control in patients with type 2 diabetes treated with basal insulin: a randomized clinical trial. JAMA, 325(22), 2262-2272. https://doi:10.1001/jama.2021.7444 Orem, D. E., & Calnan, M. E. (1972). NURSING. Nursing Management (Springhouse), 3(1), 43-46. https://doi.org/10.1097/00006247-197201000-00013 Root, A., Connolly, C., Majors, S., Ahmed, H., & Toma, M. (2022). Electronic blood glucose monitoring impacts on provider and patient behavior. Journal of the American Medical Informatics Association. https://doi.org/10.1093/jamia/ocac069 Skinner, T. C., Joensen, L., & Parkin, T. (2020). Twenty‐five years of diabetes distress research. Diabetic Medicine, 37(3), 393-400. https://doi.org/10.1111/dme.14157. |
| Grading Rubric |

Don’t wait until the last minute
Fill in your requirements and let our experts deliver your work asap.